Ostomy FAQ

Take a look at some of the most frequently asked questions (FAQ) about living with an ostomy. Still have questions
Ostomy FAQs
What is an ostomy?
One of the most common FAQs about an ostomy starts with this. What exactly is an ostomy? 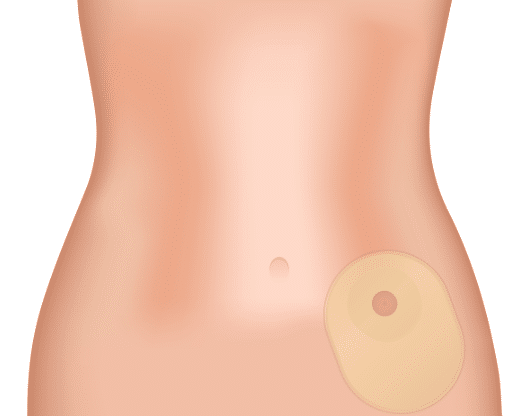
An ostomy is the surgical creation of an artificial opening known as a stoma. This artificial opening helps divert the flow of bodily waste.
What kinds of ostomies are there? It depends on why the ostomy is needed and where the surgeon creates the opening.
- Colostomy (from the colon to divert the flow of formed stool)
- Ileostomy (from the ileum, or small intestine, to divert the flow of loose stool)
- Urostomy (from the urinary system to divert the flow of urine)
Ostomies may be medically necessary due to chronic illness, cancer, an injury, or another reason. For example, people who get a colostomy or ileostomy commonly do so because of living with severe Crohn’s disease or ulcerative colitis, which are forms of IBD (inflammatory bowel disease). Someone with bladder cancer might undergo a urostomy procedure.
What does a stoma look like?
Once it heals after surgery, your stoma may slightly protrude from the abdomen. Sometimes, it heals flush with the skin, or it may recess. Its appearance should look moist and reddish-pink.
If your stoma begins bleeding excessively or changes colors, please see your treating physician as soon as possible.
Will my stoma hurt?
No, once it heals, your stoma should not cause any pain. If you feel excessive pain or experience unusual irritation, you should seek medical attention.
The stoma is connected to a pouch, which will serve as the depository for any urine or stool collected throughout the day from your ostomy.
What will my ostomy (stomal) output look like?
If you have a colostomy, your waste will typically be firm or formed stool.
An ileostomy will typically make your feces looser or even liquid.
If you have a urostomy, your urine will most likely look the same as it did before your procedure.
As far as the average amount of output, talk to your treating physician. This will depend on factors such as your individual body type, surgery type, fluid intake, and diet.
Why would you get an ostomy?
There are a variety of reasons why someone may need to have an ostomy performed.
The human body has complex systems with multiple organs that all work together for normal waste processing and elimination. Every organ along the way, from the mouth and esophagus down to the stomach, liver, and kidneys, and intestines all play a role in absorbing nutrients, eliminating toxins and waste, and processing it to leave the body.
When something hinders the normal processes of the body, whether due to a disease, illness, or injury, an ostomy surgery may be required in order to keep the body healthy and functioning.
Ostomies can be permanent or temporary, depending on the individual’s situation and condition.
Here are some of the most common reasons why someone may have to get an ostomy:
- Crohn’s disease
- Inflammatory Bowel Disease
- Bladder cancer
- Colorectal cancer
- Ulcerative colitis
- Diverticulitis
- Bladder cancer
- A blockage in the bowel
- A serious infection
- An injury to the bowel or bladder
What kind of ostomy supplies should I use?
Each case is unique to the individual. However, you can count on needing to use the basics, typically including an ostomy bag and a skin barrier. The skin barrier adheres to the skin, and the pouch then adheres to the skin barrier while collecting body waste.
One-Piece Ostomy Bags
If you prefer an all-in-one ostomy pouch, you may want to try a one-piece ostomy bag. Rather than being separate, the skin barrier and pouch come already pre-attached. Therefore, each time you change your pouch, you must remove the entire pouching system, including the skin barrier. Some people find these more convenient since they involve fewer steps and product parts.
See below for a few examples of the many one-piece pouching products at 180 Medical.
Two-Piece Ostomy Pouching Systems
A two-piece ostomy pouch has two separate components: the ostomy pouch and the skin barrier. One of the benefits of using a two-piece system is that it may be a little easier on your skin since you can change the pouch several times without removing the adhesive barrier from your skin. This may be ideal, especially if you are prone to experiencing peristomal skin irritation.
These are some of the wide variety of two-piece ostomy products available at 180 Medical.
Each person may require different types of ostomy products due to the variety of outputs. For example, someone with a colostomy will have a firmer, more fully formed stool, while someone with an ileostomy may have more liquid stool. Therefore, one person may need or prefer a closed-end ostomy pouch, while another may need a drainable ostomy pouch option. On the other hand, someone with a urostomy will need a drainable urostomy pouch to collect their urine throughout the day.
As you might imagine, there are many options out there. 180 Medical’s Ostomy Specialists can help you navigate the many ostomy product options available. We can also help troubleshoot issues like leakage or adhesive build-up with certain solutions, such as adhesive remover wipes or ostomy seals.
Here are a few of the high-quality ostomy accessories we offer at 180 Medical to complement your current pouching routine.
How do I know which ostomy products are right for me?
With the guidance of your prescribing healthcare professional, you can find the right regimen and basic product types that will work best for your particular situation.
No one product or system works for everyone since each situation and body type is unique. For instance, stoma size and protrusion, skin condition, ostomy type, and personal preferences will all need to be considered when determining the right products for you.
At 180 Medical, we’re knowledgeable about the newest ostomy supplies available and the tried-and-true products that have stood the test of time. Our Ostomy Specialists can help evaluate your options and even give you a few samples to try so you can be confident about what items you will receive before you place the full order.
Will I be able to live a normal life with an ostomy?
Lastly, this is another one of the most common FAQs about an ostomy. We’re happy to tell you yes! Plenty of people across the world live totally normal lives with their ostomies. People with ostomies can live full lives, from going to work or school to playing sports.
Of course, you’ll have to learn how to apply and change your ostomy pouch. You’ll also have to take care of the skin around your stoma to ensure it doesn’t get infected or irritated. However, the rest of your day-to-day life will likely be normal.
Talk to your doctor about any other precautions or dietary changes you may need to make. Also, wait to get back into exercising after ostomy surgery until your doctor clears you for physical activity.
Also, keep in mind that ostomy issues do happen sometimes. For example, your product needs may change over time, especially while healing after a recent ostomy surgery. Your body size and shape could change, your stoma could settle, and more. So, occasionally, you may need to update the size or shape of your products.
If you notice that your ostomy pouching system isn’t working as it should (not fitting correctly, leaking, causing skin irritation), you may want to discuss this issue with a healthcare professional.
At 180 Medical, we have direct access to a team of trained WOC (Wound, Ostomy, and Continence) nurses who can help with any questions. Give us a call, and we’ll get you connected. Often, the solution is simple, and an easy size change or accessory addition to your regimen may solve your problem.
How do I start getting ostomy supplies?
Now, how and where do you start when it comes to getting high-quality ostomy supplies and accessories? Contact 180 Medical.
We’ll gladly take care of your ostomy supply needs so you can get back to living the life you love.